In a recent study published in the journal nutrients, a team of researchers in Australia performed a review to understand the diversity of the gut microbiome at the species level and its role in the pathology of Alzheimer’s disease. They also examined how confounders such as prebiotics and probiotics and diet affect the different stages of Alzheimer’s disease.
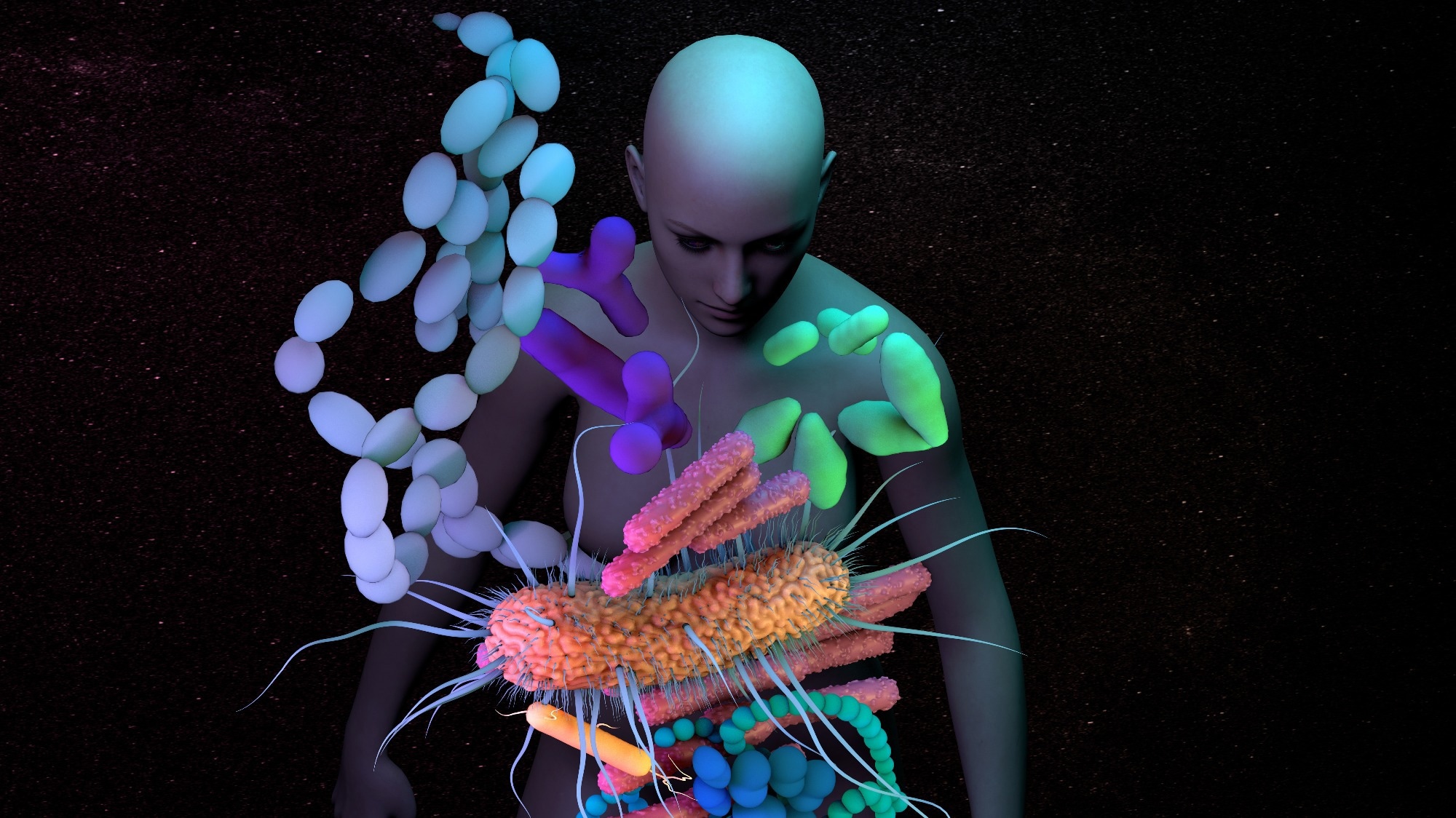 Study: The role of diet and gut microbiota in Alzheimer’s disease. Image credit: Design_Cells / Shutterstock
Study: The role of diet and gut microbiota in Alzheimer’s disease. Image credit: Design_Cells / Shutterstock
Background
Alzheimer’s disease is a neurodegenerative disease characterized by progressive cognitive impairment that affects daily life and functioning. These cognitive impairments affect abilities such as decision making, memory, problem solving, thinking and mobility, often accompanied by drastic changes in personality. Cognitive decline is due to the formation of amyloid-beta plaques and hyperphosphorylation of tau neurofibrillary tangles, which also leads to inflammation.
Recent studies have also found that the gut microbiome-brain axis plays a vital role in influencing the risk of mental disorders such as depression and various neurodegenerative diseases, including Alzheimer’s disease. Individuals with mild cognitive impairment and Alzheimer’s disease were found to have lower diversity indices for the gut microbiota compared to healthy controls.
Various factors such as age, genetics, diet, and antibiotic use are known to influence the gut microbiome, and understanding the interactions between these factors, the gut microbiome, and its potential links to Alzheimer’s disease may help identify individuals at risk early on. disease development.
Alzheimer’s disease and the gut microbiota
In the current review, researchers discussed the incidence of Alzheimer’s disease worldwide and in Australia. They also shed light on the incidence rates of dementia and dementia in young adulthood and the mortality risk associated with dementia. Studies from the United States (US) indicate that the annual healthcare costs associated with Alzheimer’s disease and dementia are over US$600 billion and are expected to increase significantly by 2030.
The review also covers what is known about the pathology of Alzheimer’s disease, including detailed discussions of the formation of amyloid-beta plaques in the brain, beginning in the orbitofrontal, temporal, and basal regions of the neocortex and eventually spreading to the amygdala, basal ganglia, the hippocampus, and the diencephalon.
Numerous hypotheses have been put forward to explain the mechanisms by which amyloid-beta peptides and tau neurofibrillary tangles contribute to neurodegeneration in Alzheimer’s disease, such as hyperphosphorylation of tau neurofibrillary tangles and the amyloid cascade. The review expanded on these hypotheses as well as other potential mechanisms such as mitochondrial dysfunction, oxidative stress and neuroinflammation.
Studies investigating the relationship between gut microbiota and Alzheimer’s disease have reported an association between specific gut microbes and different levels of Alzheimer’s biomarkers in the cerebrospinal fluid. Other studies have found a link between the composition of the gut microbiome and levels of amyloid peptide in the brain. The researchers presented an in-depth discussion of existing research on the links between specific gut microbes and various pathological aspects of Alzheimer’s disease.
Diet, gut microbiome and Alzheimer’s disease
The fact that diet plays a key role in influencing the composition and diversity of the gut microbiome is a well-supported finding. The composition of the gut microbiome may also be modified by specific dietary patterns and the consumption of various supplements, which in turn may impact the gut-brain axis and influence the pathology of Alzheimer’s disease.
The review extensively discusses the role of different dietary components such as protein, fiber, fat and polyphenols and different dietary patterns in influencing the gut microbiome environment and composition. He also reported on studies that found significant improvements in cognitive function in Alzheimer’s patients following specific dietary patterns such as the ketogenic diet, the Mediterranean diet, and diets targeting hypertension and neurodegeneration.
The researchers also found that although the amount of research on the use of pre- and probiotic supplements as therapeutic options for Alzheimer’s disease is still limited, various studies have reported that the use of pre- and probiotics and combinations of the two can alter progression of Alzheimer’s disease and related neuropathology.
Conclusions
To summarize, the review comprehensively examines existing research on the interaction between diet, gut microbiota and Alzheimer’s disease pathology. The findings suggest that gut dysbiosis is closely related to the progression of Alzheimer’s disease pathology and represents a potential avenue for non-invasive therapy and risk modification.
Journal reference:
- Dissanayaka, DM Sithara, Jayasena, V., Rainey-Smith, SR, Martins, RN, & Fernando, WMADB (2024). The role of diet and gut microbiota in Alzheimer’s disease. nutrients, 16 (3). DOI 10.3390/nu16030412, https://www.mdpi.com/2072-6643/16/3/412
