Since the 1970s, modern antibiotics have been in a lull. The World Health Organization has now named the antimicrobial resistance crisis one of the top 10 global public health threats.
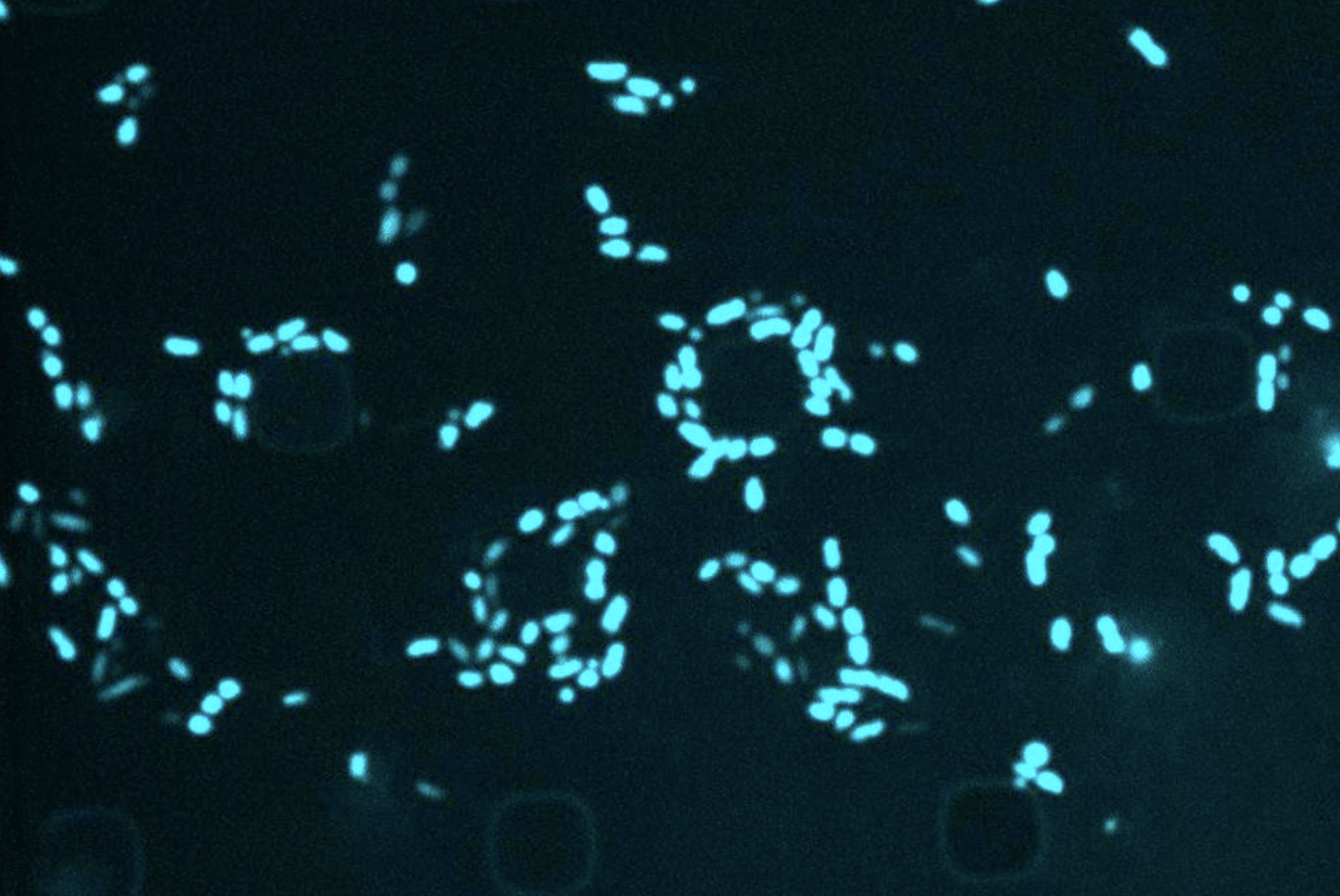
When an infection is treated repeatedly, clinicians risk bacteria becoming resistant to antibiotics. But why would the infection return after appropriate antibiotic treatment? One well-documented possibility is that the bacteria become metabolically inert, evading detection by traditional antibiotics that respond only to metabolic activity. When the danger is over, the bacteria come back to life and the infection reappears.
“Resistance builds up over time, and recurrent infections are due to this passivity,” says Jackie Valery, a former MIT-Takeda fellow (with a center at the MIT Abdul Latif Jameel Clinic for Machine Learning in Healthcare), who recently earned his PhD in biological engineering from the Collins Lab. Valerie is the first author of a new article published in this month’s issue of Cell Chemical Biology which demonstrates how machine learning can help screen for compounds that are lethal to latent bacteria.
Tales of the resilience of bacterial “sleepers” are hardly news to the scientific community—ancient bacterial strains dating back 100 million years have been found in recent years alive in an energy-conserving state on the Pacific seafloor.
MIT Jameel Clinic Life Sciences Faculty Chair James J. Collins, the Termeir Professor of Medical Engineering and Science at MIT’s Institute of Medical Engineering and Science and Department of Biological Engineering, recently made headlines for using AI to discover a new class of antibiotics, which is part of the larger mission of group to use AI to dramatically expand the existing antibiotics available.
According to a document published by The lancetin 2019, 1.27 million deaths could have been prevented if infections were susceptible to drugs, and one of the many challenges facing researchers is finding antibiotics that are able to target metabolically inactive bacteria.
In this case, Collins Lab researchers used AI to speed up the process of finding antibiotic properties in known drug compounds. With millions of molecules, the process can take years, but researchers were able to identify a compound called semapimod in a weekend thanks to AI’s ability to perform high-throughput screening.
An anti-inflammatory drug commonly used for Crohn’s disease, the researchers found that semapimod was also effective against stationary phase E. coli and Acinetobacter baumannii.
Another breakthrough was semapimod’s ability to disrupt the membranes of so-called “gram-negative” bacteria, which are known for their high intrinsic resistance to antibiotics due to their thicker, less permeable outer membrane.
Examples of Gram-negative bacteria include E. coli, A. baumannii, Salmonellaand Pseudomonisall of which are challenging to find new antibiotics.
“One of the ways we understood the mechanism of sema [sic] was that its structure was really big and it reminded us of other things that target the outer membrane,” Valerie explains. “When you start working with very small molecules … to our eyes, it’s a pretty unique structure.”
By disrupting a component of the outer membrane, semapimod sensitizes gram-negative bacteria to drugs that are normally active only against gram-positive bacteria.
Valerie recalls a quote from a 2013 post Trends in Biotechnology: “For gram-positive infections we need better drugs, but for gram-negative infections we need all kinds of drugs.”