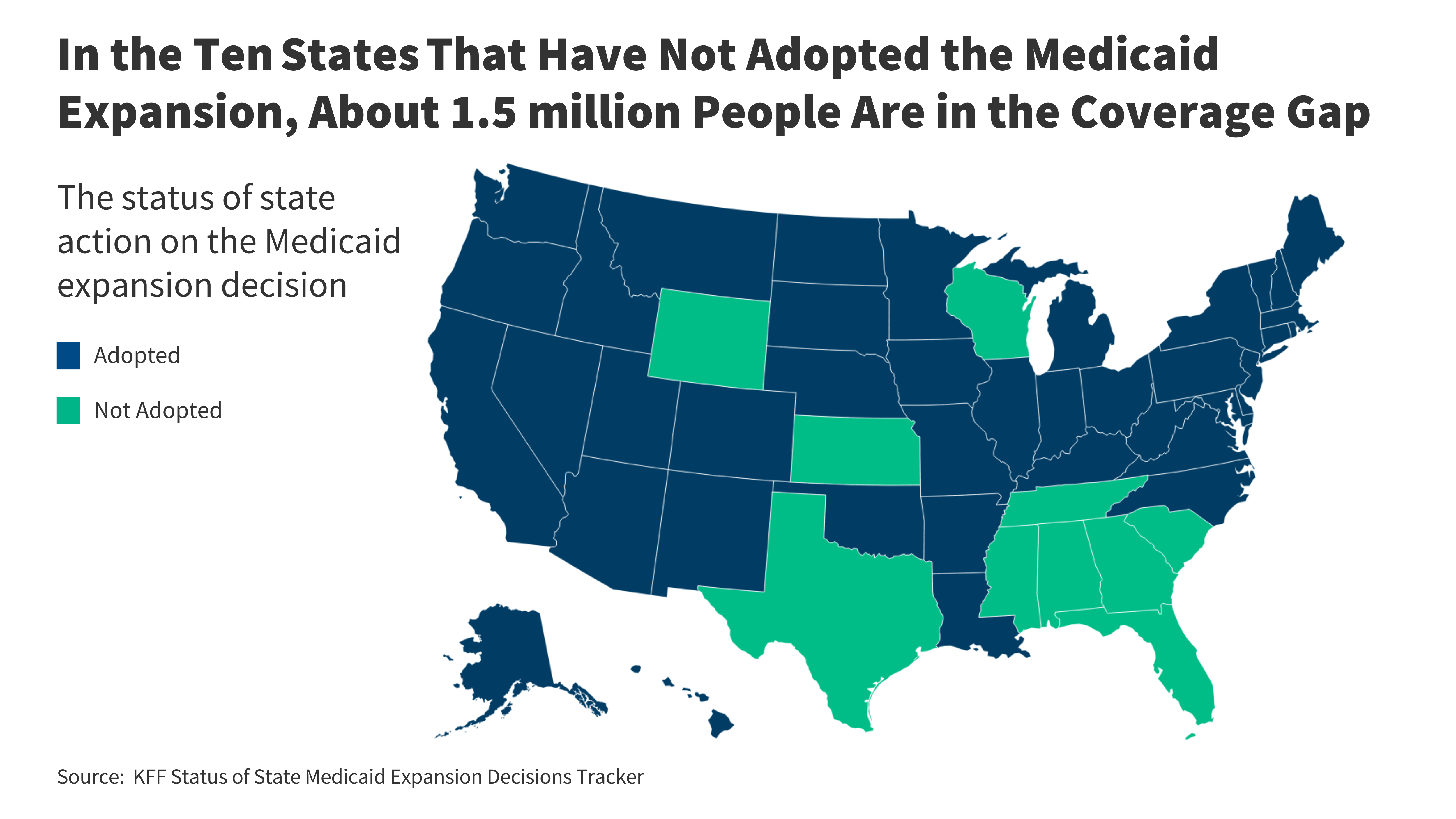
Ten years after the Affordable Care Act (ACA) coverage options were enacted, ten states have not passed the Medicaid expansion, leaving 1.5 million uninsured people without an affordable coverage option. The rollout of Medicaid’s continuous enrollment provision, along with continued financial struggles among rural hospitals, has drawn attention to gaps in Medicaid coverage in non-expansion states, and the availability of temporarily enhanced federal funding for states that recently adopted the expansion has renewed discussions to expand in some of these states.
Two states (South Dakota and North Carolina) implemented Medicaid expansions in 2023, reducing the number of low-income uninsured people nationwide without access to Medicaid. The expansion in these two states brings to 40 states and the District of Columbia that have adopted the expansion, leaving ten states that have not. Using data from 2022, the most recent year available, this brief presents projections of the number and characteristics of uninsured people in the ten non-expansion states who could be reached by Medicaid if their states adopted Medicaid expansion. An overview of the methodology underlying the analysis can be found in the Data and Methods, and more details are available in the Technical Appendices.
What is the difference in coverage?
The coverage gap exists in states that have not adopted the ACA’s Medicaid expansion for adults who are ineligible for Medicaid coverage or marketplace subsidies. The ACA expanded Medicaid to non-elderly adults with income up to 138% FPL ($15,060 per year for an individual in 2024) with enhanced federal funds (now 90%). The Medicaid expansion established a uniform eligibility threshold across states for low-income parents and newly created Medicaid coverage for adults without dependent children. However, the expansion is not effectively mandatory for states due to a 2012 Supreme Court decision. As of February 2024, 40 states and the District of Columbia had expanded Medicaid (Figure 1).
In the others ten countrieswho did not accept the Medicaid expansion, approximately 1.5 million individuals fall into the coverage gap. Adults who fall into the coverage gap have incomes above their state’s Medicaid eligibility but below poverty, making them ineligible for subsidies in the ACA Marketplaces (Figure 2). When it went into effect, the ACA did not anticipate that states would be allowed to opt out of Medicaid expansion; as such, Marketplaces subsidies are not available to people with incomes below the poverty line.
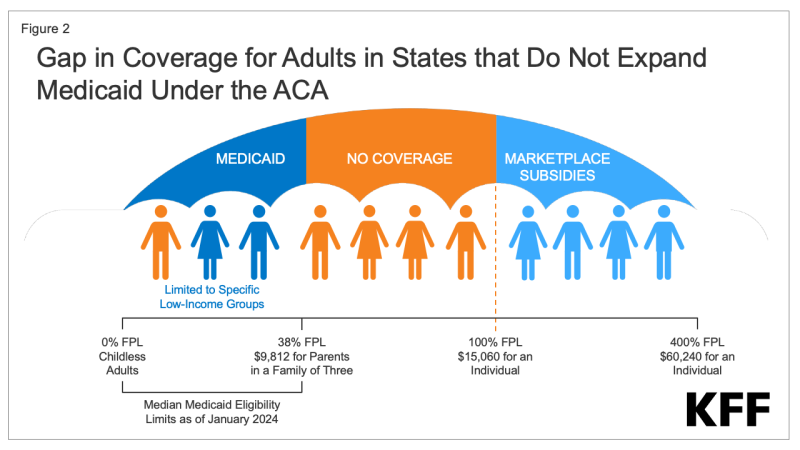
Figure 2: Difference in coverage for adults in states that did not expand Medicaid coverage under the ACA
Eligibility for Medicaid for adults in countries that have not expanded their programs is very low. In these states, the median income limit for parents is just 38% FPL, or an annual income of $9,812 for a family of three in 2024, and in almost all non-expansion states (except Wisconsin through an exemption), childless adults remain ineligible regardless of their income (Figure 3). In Texas, the state with the lowest eligibility threshold, parents in a family of three with incomes above $4,131 a year, or just $344 a month, are ineligible for Medicaid. Because there is no path to coverage for adults without children except in Wisconsin, more than three-quarters (79%) of people in the coverage gap fall into this group.
Countries that did not implement the expansion did so uninsured rates which are almost double the rate of expansion (14.1% compared to 7.5%). People without insurance coverage have worse access to care than people who are insured. One in five uninsured adults in 2022 missed out on needed medical care because of costs, and uninsured people are less likely than those with insurance to get preventive care and services for serious health conditions and chronic diseases.
What are the characteristics of people in the coverage gap?
Nearly three-quarters of adults in the coverage gap are concentrated in three states in the South. Four out of ten people in the coverage gap live in Texas, which has very limited Medicaid eligibility and therefore a large uninsured population (Figure 4). An additional 19% of people in the coverage gap live in Florida and 12% live in Georgia. A total of 97% of those in the coverage gap live in the South. Seven of the 16 states in the South have not passed Medicaid expansion, and the region has more low-income, uninsured adults and higher uninsured rates than other regions.
People in the coverage gap are disproportionately people of color. Nationally, more than six-in-ten (62%) people in the coverage gap are people of color, a share that is higher than for non-expansion adults generally in non-expansion states (53%) and for non-expansion adults nationwide (46 %) (Figure 5). These differences partly explain continuing disparities in health insurance coverage by race/ethnicity.
Although they have low incomes, nearly six in ten people in the coverage gap are in a family with a worker, and over four in ten are self-employed (Figure 6). Adults who work may still have incomes below poverty because they work low-paying jobs. People with below-poverty incomes often do not have access to employer-based health insurance, or if they do have it, it is often unaffordable. The most common occupations among adults in the coverage gap are cashier, cook, waiter/waitress, construction worker, maid/cleaner, retail salesperson, and janitor. For parents in non-expansion states, even working part-time can make them ineligible for Medicaid.
Some people in the coverage gap have significant ongoing health care needs. KFF’s analysis of the 2022 American Community Survey shows that more than one in six (17%) people in the coverage gap have a functional disability, meaning they have severe difficulties with hearing, vision, cognitive functioning, mobility , self-care or independence alive. Even with functional disabilities, many cannot qualify for Medicaid through the disability pathway, leaving them uninsured. Seniors aged 55-64, an age with increasing health care needs, make up 18% of people in the coverage gap. Research shows that uninsured people in this age group may leave their health needs untreated until they become eligible for Medicare at age 65.
How many uninsured could gain coverage if all states adopted the expansion?
If all states adopt the Medicaid expansion, an estimated 2.9 million uninsured adults will become eligible for Medicaid. This number includes 1.5 million adults in the coverage gap and an additional 1.4 million uninsured adults with incomes between 100% and 138% FPL, most of whom are currently eligible for Marketplace coverage but are not enrolled (Figure 7 and Table 1). Most of the seniors currently eligible for Marketplace coverage qualify for zero-premium plans; however, even without premiums, Medicaid can provide more comprehensive benefits and lower cost sharing than Marketplace coverage. The potential number of people who could be reached by expanding Medicaid varies by state.
What is the outlook going forward?
A substantial body of research continues to point to largely positive effects of Medicaid expansion. The KFF reports, published in 2020 and 2021, reviewed more than 600 studies and concluded that expansion is associated with gains in coverage, improved access and health, and economic benefits for states and providers. More recent studies generally find positive effects associated with more specific outcomes such as improved access to care, treatment and outcomes for cancer, chronic disease, sexual and reproductive health, and behavioral health. Studies also point to evidence of reduced racial disparities in coverage and access, reduced mortality, and improvements in economic impact for providers (especially rural hospitals) and economic stability for individuals.
The American Rescue Plan Act (ARPA) included a temporary fiscal stimulus for states that recently implemented Medicaid expansion. Under ARPA, states that recently adopt an expansion are eligible for an additional five percentage point increase in the state’s traditional matching rate (FMAP) over two years. This incentive does not apply to the growing population; states are required to cover 10% of Medicaid expansion costs, with the federal government covering 90%. Traditional FMAP applies to most costs for all groups without expansion (children, parents and eligible people over 65 or disabled); Medicaid spending for non-expansion groups is much greater than spending for the expansion group. KFF’s analysis shows that all non-enlargement countries could see a net fiscal benefit over a two-year period if they accepted enlargement. For the two states that recently adopted the expansion, South Dakota and North Carolina, the expected fiscal benefit is $60 million and $1.2 billion, respectively.
Renewed debates over Medicaid expansion may lead to the adoption of the expansion in additional states. Legislative opposition to the expansion may be waning in some states, driven by financial challenges facing rural hospitals as well as interest in taking advantage of additional federal funding. If additional states expand Medicaid, it could help limit the increase in the number of people who become uninsured due to the repeal of the Medicaid continuous enrollment provision. In South Dakota and North Carolina, Medicaid enrollment initially declined after the rollout began, but began to increase again after each state’s Medicaid expansion was implemented.